Message from the Program Director
Congratulations to those nearing the next stage of medical training and pursuing a residency in Pediatrics! I welcome you to engage in this site to learn more about the heart and aloha of our University of Hawai`i Pediatric Residency program in Honolulu, Hawai`i.
We have a wonderfully unique learning environment as Kapi`olani Medical Center for Women and Children is the only tertiary care pediatric referral center in the Pacific Basin. Our health care system serves not only families from the Hawaiian Islands but also families in our neighboring territories and Pacific Island countries as well as visitors here on vacation.
Our residents see patients with a wide variety of common pediatric diagnoses, patients with rare diseases including tropical medicine problems and patients presenting in all stages of illness. Our main training site is an urban, university-affiliated, community hospital with a bustling census and we also have opportunities for rotations in rural and resource-limited settings. The three years of pediatric residency in our program offer an incredible experience of growth and professional development as young physicians mature into competent pediatricians. It is expected to be a challenging time as knowledge is expanded and abilities are stretched while residents learn how to provide the best in evidence based, effective care.
Working with our patients and their families is a gift, and we are grateful that our local community values our training program. Their support of residents caring for their keiki is crucial as our residents develop their clinical acumen. Residency is a time of great camaraderie, with many of our residents building sustaining relationships that are a source of strength and peer mentorship throughout their professional careers. While learning how to provide consummate care of pediatric patients, residents also cultivate valuable skills in providing successful leadership of a team, developing and practicing empathy, providing succinct, clear communication and in considering the whole patient and family when making management decisions together.
It truly “takes a village” to raise a successful pediatrician, and our faculty are exceptionally invested in the success of our residents and program through their clinical precepting, lectures, advising and research mentorship. We have a remarkable team, including nurses and staff who all help our residents grow.
I wake up every day feeling grateful for the privilege of directing this incredible residency program.
Aloha,
Dr. Jennifer Di Rocco
University of Hawai`i Pediatric Residency Program Director

In 1890 Queen Kapiolani founded the Kapiolani Maternity Home to care for Hawaii’s mothers and babies. The hospital later merged with Kauikeolani Children’s Hospital in 1978 to become Kapiolani. We are honored to work and learn at Kapiolani Medical Center for Women and Children, literally carrying on the legacy of the beloved Queen Kapiolani.
For more information, visit:
Kapiolani Medical Center Women and Children Webpage
Program Leadership & Administrative Staff
Program Details
Curriculum
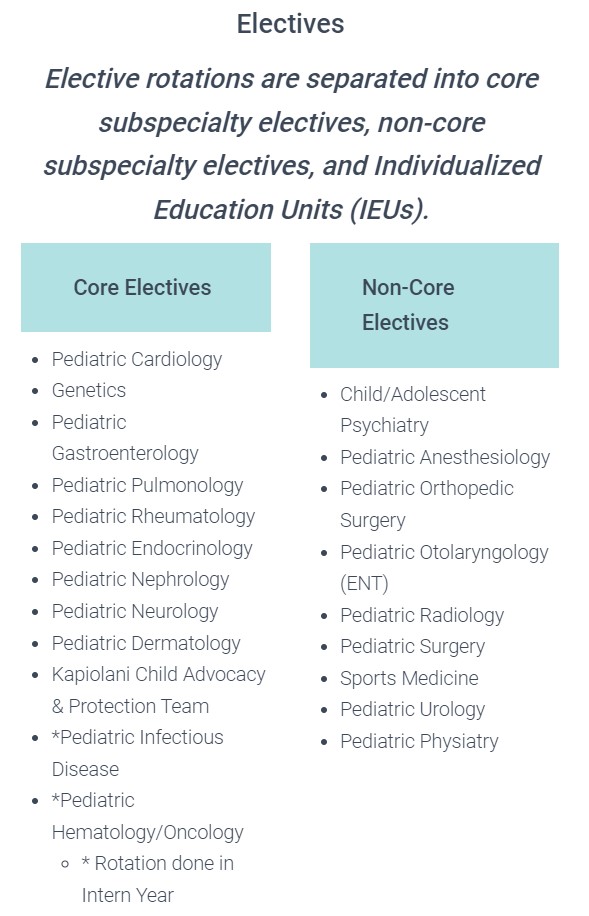
University of Hawai’i Pediatric Residency Curriculum
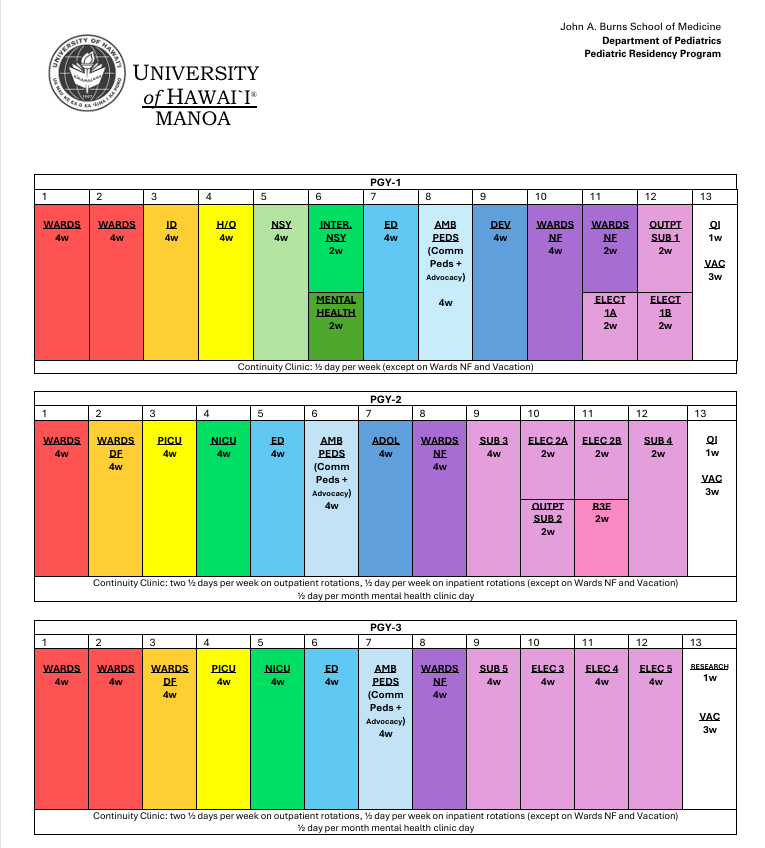
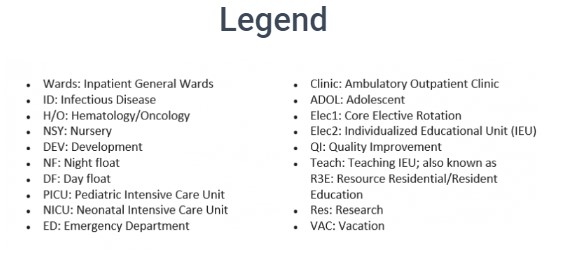
Our overall schedule is comprised of 13 four-week blocks, with one block being assigned as call free each year. There are 3 weeks of vacation each year, split into 2wks and 1 wks. As a resident progresses toward the PGY 3 year, the curriculum incorporates more elective time, supporting an educational platform that fits each person’s educational trajectory and goals.
“This curriculum applies to residents starting in July 2025 and subsequent years”
Meet our awesome core rotation directors! Below is a message or summary of the required core rotations in our residency program.

Hematology & Oncology
Darryl Glaser, M.D
The 4-week Pediatric Hematology and Oncology rotation allows PGY-1 residents the chance to take care of an amazing group of patients and families who may be dealing with unique issues including learning of and living with a life-threatening diagnosis, end of life care, palliative care and symptom control. There is a wide range of acuity on the rotation, with some patients showing no signs of illness and others who are extremely or critically ill. Multidisciplinary care is key in oncology, and the resident will be an integral part of this comprehensive team. Their primary responsibility will be to lead the team in caring for hospitalized heme-onc patients, with direct support from their attending physician, but they will also have the opportunity to act as a consultant for other services that have patients with hematologic problems. Residents will also have the opportunity to perform lumbar punctures and bone marrow aspirations on sedated patients. During this rotation, residents gain the knowledge and experience that allows them to confidently take care of the heme-onc population when they rotate through night float later in the year.

Ambulatory
Lindsey Heathcock, M.D.
Ambulatory Pediatrics is part of a continuum of rotations/experiences designed to expand resident comfort and competence in managing patients and supporting families in the outpatient setting. Topics in ambulatory pediatrics are covered in residents’ continuity clinics, Developmental Behavioral Rotation, Adolescent Rotation and this rotation. 4 weeks are spent in each of the 1st, 2nd and 3rd years of residency primarily in the Kapiolani Medical Center for Women and Children Pediatric Outpatient Department (KMCWC). During the first year, experiences are chosen and common to all, such as orientation to topics in advocacy, child abuse, sex abuse treatment center etc. Experiences can be expanded based on particular interests or learning goals. During the 2nd and 3rd year, time away from clinic can be chosen similar to IEU (Individual Educational Units) based on individual learning needs and objectives. There is flexibility to participate in home-, school-, community-based or other educational opportunities.
PICU
Prashant Purohit, M.D.
The PICU at KMCWC is a 14 bed multidisciplinary intensive care unit, and is the primary tertiary referral center for the sickest children from community hospitals on O’ahu and neighboring islands. You will care for the cases ranging from “simple” single system failure to patients requiring ECMO – extracorporeal membrane oxygenation. We also manage active surgical patients including those with trauma, airway surgeries, orthopedic surgeries, neurosurgical patients requiring ICP monitoring, patients requiring continuous renal replacement therapy, continuous EEG monitoring and so forth. Sepsis, pneumonia and airway obstruction requiring medical and surgical interventions are the other commonly encountered patients in our PICU. We also manage post bone marrow/stem cell transplant patients in the PICU in case of any complications.
Residents do their first PICU rotation in their second year and the second rotation as third year. Usually there are two residents at a time and routinely one resident is from University of Hawai‘i Pediatric Residency Program and another resident is from Tripler Army Medical Center. We often have a third or a fourth-year medical student doing their rotation with us. There will be numerous opportunities to do procedures such as endotracheal intubation, bag-mask ventilation, peripheral intravenous and arterial line placement, chest tube placement and so forth. The PICU rotation is popular for learning diverse physiology, disease processes, autonomy and procedures!

Wards
Gina Ramirez, M.D.
The inpatient wards rotation is comprised of three separate experiences on the pediatric units of Kapiolani Medical Center for Women and Children: the wards team, day float, and night float. On this busy and deeply rewarding rotation, you will have exposure to both “bread and butter” pediatrics and highly complex patients, allowing you to develop your critical thinking skills in the acute and chronic care of hospitalized pediatric patients.
The wards team is a 4-week rotation, while day float and night float are each 2-week rotations. As a PGY1, you will rotate twice through the wards team and three times through night float. As a PGY2, you will be the wards team senior for one block, and rotate through night float and day float twice each. As a PGY3, you will have two blocks as a wards senior, and six weeks of a combination of day float and night float. On the wards team, you will be the primary physician for 6-8 patients every day and participate in Patient and Family-Centered Rounds, serving as the main point of contact for patients, families, and nurses, while performing admissions in the afternoon. On day float and night float, you will largely be focused on admitting new patients, while also performing cross-cover duties. During your time on the wards, you will work closely with MS3s, MS4s, visiting residents, a growing number of Pediatric Hospitalists (plus a small group of private PCPs), and a fantastic inter-professional team to provide exceptional care to an extremely diverse and unique patient population!

Newborn Nursery
Joan Meister, M.D.
The newborn nursery at KMCWC is the “happiest place” on earth! All your patients are cute and cuddly and chubby; well some might be scrawny and bruised and molded from entering this world—but still cute.
As an intern you will spend 4 weeks in the newborn nursery. Your patients will be newborns 35 weeks and above along with their parents. You will spend time examining them and figuring out the wide spectrum of normal. You will spend time learning vital signs and transition and when to intervene and when not to. You will circumcise the boys whose parents decide they want one; you will transfer babies who are not feeling well to the NICU; you will discharge moms and babies home knowing you have prepared them for their “new normal” You will also face the frustration of trying to educate parents who do not feel the routine newborn care such as immunizations and Vit K are important; you will feel accomplishment when you have effectively educated them. You will also feel the frustration of speaking with a mom who may be losing her child to CWS due to drug use; but you will experience the joy of seeing that even though that mom has made bad choices; she still wants to learn about her baby. You will also attend deliveries and help the tiniest and sickest babies transition to this new world. And you will do this all while teaching and mentoring 3rd year medical students.
As a 3rd year resident, you will return to the Newborn nursery for 2 weeks. You will be responsible for teaching the intern and medical students and running the service; running rounds; and supervising the care of the patients on the service. You will also gain confidence in seeing that although you haven’t been in the nursery for 2 years—you have acquired the skills and knowledge base to function in any area of pediatrics. You will see that you are ready to be a full-fledged practicing pediatrician.
Infectious Disease


A detailed and comprehensive knowledge of the diagnosis, treatment and prevention of Infectious Diseases (ID) is essential for the pediatrician in every field of practice. This rotation, coming as it does in the first year of pediatric residency, is designed as an introduction to the field. Our overall objective is to focus on principles of evidence based medicine where it exists and to encourage a scholarly approach to all ID problems in order to:
- Increase the resident’s specific current medical knowledge
- Develop skills in medical communication
- Develop diagnostic and therapeutic reasoning skills.
Residents will work as part of a team with the ID Attending physician(s) and others who often rotate with the ID Attending Physicians including undergraduate students, medical students, nurse practitioner students and residents from other programs.
Emergency Medicine
Travis Hong, M.D.
Residents rotate through the Pediatric Emergency Department for one month in each of the three years. The ED is an exceptional location to learn to take care of patients with a wide variety of complaints and acuity levels, ranging from simple viral illnesses to bread and butter pediatric problems to major trauma. It is a fast-paced and exciting learning environment where you will be the patient’s primary healthcare provider. Here it is all about a wide breadth of learning experience!
You will work with as an integral part of a team that includes our incredible attending physicians, your resident peers, and medical students.
Welcome to Hawaii and I’m looking forward to working with you in the near future!

NICU
Melanie Snyder, M.D.
The neonatal intensive care unit (NICU) at Kapiolani Medical Center for Women and Children (KMCWC) specializes in the care of premature newborns and infants requiring intensive or telemetry level care. The NICU medical team is staffed by neonatologists, neonatal hospitalists, neonatal nurse practitioners (NNPs), neonatal fellows, pediatric residents, and medical students. With an average daily census of 72 infants, the NICU maintains a level of acuity and volume (over 1100 admissions per year) on par with the busiest NICUs in the country. In addition, the neonatology division is responsible for providing neonatal coverage for high-risk deliveries and resuscitations, when necessary, for the 6000+ annual deliveries at KMCWC. We are also the primary tertiary care referral center for community hospitals on Oahu and neighboring islands. Treatment teams in the NICU are divided mainly between two high-acuity services (Pili and Pono), a medium-acuity service (Pāola), a low to medium-acuity and delivery service (Pūlama), and one low-acuity teams (Pōmaika’i).
The focus of the NICU experience is to prepare a general pediatrician to care for the high-risk neonate. This includes stabilization of the newborn infant in the delivery room, identifying neonates who require monitoring and treatment beyond the delivery room or transitional nursery, transitioning NICU infants to home and the community, and understanding issues that will require ongoing management as outpatients.

Developmental Pediatrics
Jeff Okamoto, M.D.
The Developmental Pediatrics rotation is a rotation where residents focus on normal infant and child development and milestones as well as abnormal developmental disorders through direct clinical experiences. The rotation is done once in the PGY 1 year.

Adolescent
Pia Francisco-Natanauan, M.D.
The four-week block rotation in Adolescent Medicine (done in the PGY2 year) provides medical trainees with an experience that will enable them to recognize the spectrum of normal and abnormal growth and development during the adolescent years. It is primarily ambulatory and community-based. It also provides knowledge and skills that can be applied in the medical trainee’s work with adolescents in a variety of in-patient, ambulatory, primary and specialty care settings. Residents rotate between the following clinical sites: Adolescent Clinic (at Hale Pawa’a and Tripler Clinics), Detention Home Medical Unit, and Hawaii Youth Correctional Facility Medical Unit.
Our residents have continuity clinics at either Kapiʻolani Medical Center for Women and Children, Queen Emma Clinic at Queen’s Medical Center or Kokua Kalihi Valley Community Health Center in Kalihi.
Each resident is assigned to one half‐day of clinic per week during their PGY‐1 year and two half‐days of clinic per week during their PGY‐2 and PGY‐3 years. Clinics are cancelled during vacation and night‐shift rotations for all residents. Residents do not attend the second half‐day of clinic when on inpatient rotations (ER, NICU, PICU, Wards).
Kapiolani Medical Center for Women and Children Pediatric Clinic
Resident Experience Testimonials:
“Kapiolani Outpatient Clinic serves a diverse population consisting of children with various socioeconomic backgrounds as well as serving a range of needs that includes routine well child checks and follow up for NICU graduates and complex children with neurodevelopmental disorders. Our residents work in conjunction with specialists to provide routine care with and gain exposure to children with trachs and G-tubes. Residents also get an opportunity to hone their skills in navigating translation services for families that are available in person or via phone. The beauty of care in our clinic is the continuity that our residents achieve by often serving as the primary physician for children whom they closely cared for in the Kapiolani nursery and NICU. This continuity helps foster rapport, as residents can build their own patient panel. Thus, many families see our residents both in the clinical and hospital setting, providing a sense of ownership and autonomy.”

Queen Emma Clinic at Queens Medical Center

Resident Experience Testimonials:
“Queen Emma Clinic has been one of the best parts of my time in residency. We have a busy primary care clinic serving a diverse range of patients from all over Oahu following in the mission of Queen Emma And King Kamehameha IV. QEC has great continuity, and we are able to build and maintain close relationships with our patients and families. The clinic operates with a collaborative approach, and the attendings support our ownership and follow up of patients. Though not directly, given that we are in a larger primary clinic, we often have entire families coming to QEC for their care adding to our sense of community and purpose.”

Kokua Kalihi Valley (KKV) Community Health Center

Resident Experience Testimonials:
“Kokua Kalihi Valley (KKV) is a federally qualified health center that serves the community of Kalihi within the 96819 zipcode. Our patients comprise of 93% Asian and Pacific Islander descent with many of them who speak a language other than English (including but not limited to Chuukese, Ilocano, Tagalog, and Samoan). KKV is the only community health center in the nation to have a 100-acre nature preserve as a site of healing, named Ho’oulu ‘Aina. The food and medicinal plants harvested at Ho’oulu ‘Aina are shared amongst the community through Roots Cafe, with the intention to share one’s heritage and life experiences through the dishes prepared for the community. The services offered at KKV include evidence-based medical care (pediatrics, OB-GYN, adult medicine), family planning, dental, behavioral health, in-person interpreters for appointments, WIC and nutrition counseling, and free legal advocacy clinics. What I love about KKV, apart from having an amazingly supportive attending and medical assistant staff, is the opportunity to provide a comprehensive medical home and welcoming community for our patients where they can receive most of the services they need to achieve a healthy life. Working at KKV, I am more knowledgeable about community/government funded resources that I can educate my patient’s families about so that they feel empowered to seek out these resources and take an active role in the positive development of their child’s life.”

IEU

Aloha!
We are Drs. Sood and Kurahara, the Co-Directors for Individualized Educational Units (IEUs). IEUs are a curricular concept from the ACGME that we have had in our program since 2014. These individualized rotations allow programs to help residents align their elective rotations with their own educational and career goals. Residents have 6 weeks of IEUs in their PGY2 year and 15 weeks in their PGY3 year. Each IEU rotation is crafted by collaboration between the resident, faculty advisors/preceptors, program leadership, and IEU committee; and goals and objectives are designed to help residents develop skills needed to function as an attending in the career path of their choice. Whatever you imagine yourself doing in your career, you can use IEUs to help best prepare you for this path! In our residency program, you will have a curriculum that is totally unique to you!
Global Health/International Medicine


Our residency program incorporates Global Health into all aspects of resident education. Not only do our patients hail from across the Pacific and around the world, but we go out of our way to train our residents in culturally competent care and emphasize the importance of translator use for patients or families with limited English proficiency. We collaborate with other local residency programs to offer biannual multidisciplinary academic half day sessions on Global Health topics ranging from HIV to the health effects of climate change. Over the past ten years, we have developed several 2–4-week rotations for our PGY3 residents, including rotations at Lao Friends Hospital for Children in Luang Prabang, Laos and LBJ Tropical Medical Center in Pago Pago, American Samoa. Residents can also take advantage of an opportunity to join Shriner’s orthopedic surgeons on their musculoskeletal medicine missions within the South Pacific (including to Fiji, Tonga, American and Western Samoa, and the Marshall Islands), and we hope to add a clinical experience in Palau in the near future. We have a robust pre-departure curriculum and provide ample opportunities to debrief upon return.
For more information, please do not hesitate to reach out to the Global Health curriculum co-directors: Anna-Lena Lueker, M.D. and Maya Maxym, M.D.
Applicants are invited to apply to our program through the Electronic Residency Applications System (ERAS) from the start of the ERAS and National Resident Matching Program (NRMP) season, through December 1st. Applications submitted after December 1st will not be reviewed. All communication regarding residency selection will be done via ERAS or Thalamus GME Interview Schedule platform.
All applications need to include:
- At least three letters of reference (at least one from a pediatrics rotation)
- Medical Student Performance Evaluation Letter (MSPE)
- Personal Statement
- Curriculum vitae/ERAS common application
- Full medical school transcript
- USMLE or COMLEX transcript
- USMLE is not required for Osteopathic applicants
- Step 1 scores need to be resulted to be invited for an interview
- Applications with resulted Step 2 scores will be prioritized for interview consideration
- Results from both Steps 1 and 2 are required prior to the end of the interview season (Jan 31st)
Additional information for International Medical Graduates (IMGs):
Our program sponsors J-1 visas only. IMG applicants must be ECFMG certified if they have graduated from medical school at the time of application and must be ECFMG certified by the start of Residency if they have not yet graduated.
Prior residency training is not required for our residency program, though hands-on clinical experiences in the United States are particularly valued.
Interview Season:
Interviews are by invitation only and will be conducted via a virtual platform for all applicants.We interview November through January on selected Mondays and Tuesdays, and all interview invitations are extended only via Thalamus GME Scheduler.
Miscellaneous Information:
A matched applicant’s acceptance into our program will be contingent upon verification of supporting documents and a personal background check.Should you have additional questions please contact:Recruitment and Selection Administrator, peds@hawaii.edu
Please be aware that all incoming residents are required to be fully vaccinated.
Hawaii Residency Programs, Inc. provides equal employment opportunities to all employees and applicants for employment. We do not discriminate on the basis of age, race, color, religion, gender/sex, national origin, ancestry, citizenship, disability, marital status, domestic or sexual violence victim status, arrest and court record, credit history and credit report, sexual orientation, military and veteran status, or other protects categories in accordance with state and federal laws. If you need accommodations at any time, please contact HRP Human Resources at 808-586-2891.
PGY-1 Class of 2028
PGY-2 Class of 2027
PGY-3 Class of 2026
Notable Program Benefits
-Relocation reimbursement ($2,000)
-Hospital Parking included-Paid meals on call (stipend/meal card, discount)
-Insurance (Medical, Vision, Dental, Malpractice, Disability, Life)
-Paid vacation 3 weeks per year (2 wk + 1 wk)
-Paid sick leave: 12 days per year-Annual AAP membership (includes Journal of Pediatrics, Board PREP questions)
-Up to 7 days allowed annually for educational leave in PGY2 and PGY3 years
-Educational travel stipend (up to $2,540)
-Yearly Critical Care Course (PFCCS)
-Additional grant funding available to residents for scholarly activities (research costs, poster/media printing, travel expenses)
-Reimbursement of up to $350 each year for educational materials
Below includes a summary of research expectations and resources in our program. The Accreditation Council for Graduate Medical Education (ACGME) requires that residents participate in scholarships as part of their well-rounded residency education.
Scholarships can span a variety of levels based on each resident’s specific interests and post-residency career goals. All PGY-3 residents perform a podium presentation of their scholarly work at our annual Dr. Raul Rudoy Pediatric Research Day in May.
Any one of the following activities would meet both the ACGME requirement and our program’s scholarly activity expectations for graduation:
1) Become a part of an ongoing prospective trial or a retrospective cohort analysis. Your research mentor can support your contribution for graduation with or without offering you a co-authorship.
2) Initiate your own prospective trial or chart review project.
3) Write a case report or case series with appropriate literature review and manuscript preparation (publication is encouraged but not mandatory).
4) Participate in a Quality Improvement (QI) or Advocacy Project.
Additional activities that would strengthen your scholarly activity experience/exposure:
- Submit your project for Institutional Review Board (IRB) approval (with intention to disseminate your results in abstract/poster format and/or subsequent publication).
- Apply for grant funding approval. This remains a huge challenge in the world of research in any field, even for senior researchers with a plethora of grants and publications. We don’t expect a resident to get funding approved. However, if you can, it will be considered a highly respectable aspect of your scholarship.
- Present your work at a local, regional or national conference. We will provide you with notifications of these conference opportunities as they arise.
To help support our research endeavors, residents have regular support from our Research Team, a group of invested faculty members who are actively involved in research and are enthusiastic supporters of residents in their scholarly activity. The Research Team, led by Dr. Prashant Purohit (prashant.purohit@hphmg.org), meets with residents quarterly to discuss specific goals and objectives intended to ensure each resident has the resources, tools, and support to meet the scholarly activity expectations of the program.
Research Regulations and requirements at HPH
Research at Hawaii Pacific Health – Hawaii Pacific Health
Funding resources in Hawaii
(1) Hawaii Pediatric Association Research and EducationFoundation (HPAREF)
Hawaii Pediatric Association Research and Education Foundation (hparef.org)
(2) Chun Foundation
Chun Foundation – Bank of Hawaii (boh.com)
(3) HMSA
Foundation HMSA Foundation
(4) Hawaii Community Foundation
Medical Research Grants – Hawaii Community Foundation
(5) Ola Hawaii
Ola HAWAII – Health And Wellness Achieved by Impacting Inequalities
(6) Center for Pacific Innovations, Knowledge and Opportunities (PIKO)
Center for Pacific Innovations, Knowledge and Opportunities (PIKO) – Clinical and Translational Research Infrastructure Network (hawaii.edu)
Morning Report: 30-minute case-based conference, cases are led by residents. The Morning Report schedule also includes monthly EKF and neuroradiology rounds. Here is a list of some of the topics covered in Morning Report:
- Cystic Fibrosis
- Hepatoblastoma
- Tetralogy of Fallot
- Ventricular Septal Defect
- Beckwith-Wiedemann
- Acute rheumatic fever
- Anorexia nervosa/nutritional insufficiency
- Cellulitis
- Foreign body
- Asthma
- Vocal cord cyst
- Pancreatitis
- Necrotizing enterolcolitis
- Infantile spasms
- Bronchiolitis
- Acute lymphoblastic leukemia
- Hirschsprung
- Septic arthritis
- Burkitt’s lymphoma
- Myocarditis
- MIS-C Multisystem Inflammatory Syndrome in Children
- NMDA encephalitis
- PSGN/PIGN
- Vitamin B-12 deficiency
- Hypoxic Ischemic Encephalopathy
- Concussion
- Acute kidney injury
- Precocious puberty
- Vaping-induced lung injury
- Esophageal atresia
- Biliary atresia
- Orbital cellulitis
- Hematuria
- Vitamin C deficiency
- Milk protein allergy
- BRUE- Brief Resolved Unexplained Event
- Congenital toxoplasmosis
- Diabetic Ketoacidosis
- Chronic Myelogenous Leukemia
- COVID pneumonia
- Retropharyngeal abscess
- Leptospirosis
- Henoch-Schonlein purpura/IgA Vasculitis
- SLE/Lupus
- Pseudotumor cerebri
- Duodenal web
- Rhabdomyosarcoma
- Neuroblastoma
- Duodenal atresia
- Supraventricular tachycardia
- Myasthenia gravis
- Acne
- Optic neuritis
- Nasal polyps
- Spherocytosis
- GBS meningitis
- Short stature
- UTI/pyelonephritis
- Ataxia
- Meckel’s diverticulum
- Guillain-Barre
Grand Rounds: A weekly 1-hour department wide conference, with emphasis on important and current topics related to the latest developments in pediatric care. Each resident is required to give a grand rounds presentation in their PGY3 year.
AHD (Academic Half Day): AHD is a weekly didactic session held on Wednesdays from 1230-1630. Residents are excused from clinical duties during this time.Sample AHD Schedule (JC=Journal Club)
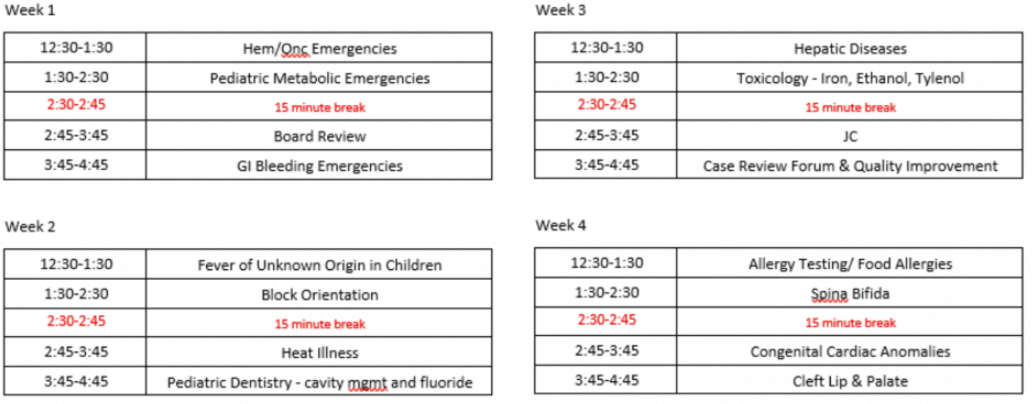
Conferences: Incorporated into Academic Half Day, residents participate in Journal Club, Case Review, and Board Review.
Simulation Lab: SimTiki sessions are held at the University of Hawaii, JABSOM (John A Burns School of Medicine), most often during some AHD sessions. Simulation sessions are also incorporated to some inpatient rotations (i.e. mock codes).
PFCCS (Pediatric Fundamentals in Critical Care Support): An annual course provided to all residents – combination of didactics and hands on sessions. Course focuses on the the ability to recognize critical illness and the fundamental management principles for the initial stabilization of a critically ill pediatric patient.
PIPPS (Pediatric Interprofessional Program): The Pediatric Interprofessional Program is a one day session that provides students from the University of Hawaii John A. Burns School of Medicine, Pediatric Residency Program, UH Manoa School of Nursing, Myron B. Thompson School of Social Work and Public Health Studies, and Pacific Health Ministry – Clinical Pastoral Education Residency Program with an opportunity to work together in an acute pediatric intensive care environment. The goal of this interprofessional education (IPE) event is for students to gain an understanding of the importance of interprofessional team collaboration to support families when providing “bad news” and exploring goals of care for pediatric clients in an acute pediatric intensive care environment.
The Cameron Kravitt Foundation Seminar on Death and Bereavement is an annual conference that allows residents to practice their communication and empathy. They experience difficult scenarios with simulated parents, learn from families who have had a child die, hear from expert speakers on post-death protocols, spirituality, and discuss physician wellness and resiliency. This seminar has expanded to include our OB/GYN and Family Medicine colleagues in a collaboration that allows residents and faculty to learn from each other across disciplines while experiencing this important topic together.
Our residents have a wide spectrum of opportunities to participate in advocacy and community involvement. These range from incorporating advocacy work into scholarly activity, spearheading a novel project to assess/meet community needs, or participating in large scale events that are hosted by JABSOM (University of Hawaii John. A Burns School of Medicine) or Hawaii Pacific Health/Kapiolani Medical Center for Women and Children.
Pediatric faculty and resident physicians lead a pediatric focused, multi-disciplinary committee that does work to enhance our ability to care for all patients and members of our communities.

Contact
Pediatrics Residency Program
1319 Punahou Street, 7th floor.
Honolulu, Hawaii 96826
Ph: (808) 369-1264
Fax: (808) 369-1212
Kapi’olani Medical Center for Women & Children
Please contact Kapi`olani Medical Center’s main line for our Faculty’s Clinical Practices and their directory at:
(808) 983-6000