A message from the Program Director
It is my privilege and honor to be the Program Director for the University of Hawai‘i Primary Care (“UHPC”) Internal Medicine Residency Program. Providing a distinct residency program specializing in primary care and ambulatory medicine enables accepted residents to participate in a unique learning experience that will provide an exceptional foundation in ambulatory medicine and general internal medicine, and provide the necessary skills to meet Hawai‘i’s unique healthcare needs.
Becoming a primary care physician is one of the most special honors that can be bestowed upon a doctor, and I am proud that this program acknowledges this fact and endeavors to train residents to not only become leaders in patient centered care, but also helps to mold compassionate, patient advocates into primary care physician champions of the future.
Dr. James Yess
Program Director
University of Hawai‘i Primary Care Internal Medicine Residency Program (UHPC) is a NEW and DISTINCT Internal Medicine Program. Having its origins as a “track” embedded within the University of Hawai‘i’s categorical Internal Medicine program, UHPC will now be a “stand-alone” program with the added flexibility and resources to truly enhance and embrace the Primary Care educational experience.
UHPC will be accepting applicants for the Fall 2024 application season, and participating in the National Resident Matching Program (“The Match”) and ERAS.
The mission of the University of Hawai‘i Primary Care Internal Medicine Residency Program is to train culturally humble physicians equipped to provide high-quality primary care to a underrepresented patient population. Graduates from the program will be prepared with the knowledge, skill set, and experience to provide primary care in various models of practice to improve the well-being of the people of Hawai‘i.
UHPC is dedicated to training physicians who treat the whole patient. Through clinical rotation design, didactic curriculum development, and the behaviors that our faculty strive to embody, UHPC espouses a biopsychosocial model of patient care, which acknowledges the intersection of the physical, mental, and social factors that play into every experience of health or disease.
We strive to learn from and embody the Native Hawaiian health model of the Lokahi Triangle. This symbol has two simultaneous representations. Within the individual, the Triangle represents balance between physical, mental, and spiritual health. On the broader scale, it asserts the interconnectedness of land (‘Aina), people and community (Kanaka), and the greater powers (Nā Aumākua).
These concepts permeate how we care for our patients as well as our residents.
Core Faculty & Staff
The University of Hawai‘i Department of Medicine is made up of a team of faculty physicians with various backgrounds, training and experience who educate the residents and fellows in both the traditional didactic setting and the clinical learning environment while providing quality primary care to the people of Hawai‘i.
Program Details
Curriculum
Flexibility to Follow Your Passion
UHPC offers great flexibility within the curriculum, allowing residents to navigate core values in the fundamental skill set while also tailoring experiences to meet their future career goals. Learn more below about the subspecialty experiences, private ambulatory rotations, and other ways UHPC nurtures its residents’ professional aspirations.
Weighted Outpatient Experiences
Internal Medicine residencies have traditionally been primarily focused on inpatient training. All Internal Medicine residencies are required to provide a minimum of 10 months of inpatient time including 2 months of dedicated critical care experience. Within these guidelines, UHPC approximates about 1/3 of the training will be inpatient focused, allowing for the overwhelming majority of training time to be situated in outpatient ambulatory settings. While providing exceptional clinical training in core General Internal Medicine topics, our program emphasizes the longitudinal relationships formed with our patients, the nuanced subspecialty education essential for Primary Care medicine, and the close-knit learning community in which our residents will be embedded.
Specialty Selectives
The UHPC curriculum emphasizes a multi-specialty ambulatory training experience, focused on the diverse exposures to consultative and ambulatory specialties that develop a well-prepared general internist.
Residents will be provided a “menu” of tailored ambulatory specialty experiences, such as Cardiology, Nephrology, Dermatology, Endocrinology, Pulmonology, Rheumatology & Musculoskeletal, Addiction, Geriatrics, and more. These rotations guarantee residents the opportunity to gain significant exposure and confidence in managing the most common outpatient problems.
Diverse Practice Model Exposure
UHPC residents will be exposed to a myriad of primary care sites, faculty, and practice models. In addition to the continuity clinic experience and the neighbor island experiences described above, UHPC residents will also have designated time to visit other primary care practices around O‘ahu. Examples include private offices, federally qualified health centers (FQHC), and the Queen Emma Clinics.
Neighbor Islands & Rural Health
Each UHPC resident will spend one month in the second year and one month in the third year at one of various primary care sites off of O‘ahu, such as our collaborating sites on the islands of Maui and Hawai‘i (“big island”). This rotation provides residents with firsthand with diverse practice models and populations across the islands, and time to learn from the outstanding physicians who proudly serve these regions of greatest need in our state. The UHPCIMRP program will cover the expense of housing and transportation to facilitate a more enriching learning experience. These opportunities allow residents to not only explore rural health across the state of Hawai‘i, but encourage the residents to be embedded culturally into the social fibers of the communities. Residents will establish holistic appreciation of rural health and further inform UHPC’s roots within the community.
Continuity Clinic and Ambulatory Blocks
A strong continuity clinic experience is at the core of the UHPC curriculum, and ample time is allotted to caring for the residents’ own primary care panel. The cornerstone of UHPC’s ambulatory training is the ambulatory immersion block. These strategically designed 4-week blocks occur three times per PGY year and include not only continuity clinics but also a combination of didactics, excursions, and/or clinical specialty experiences.
Residents also return for continuity clinic half-days during rotations such as electives and specialty selectives to ensure effective continuity of care between the residents and their personal panel of patients. Importantly, residents will be free of continuity clinic duties when on inpatient rotations, away rotations, and vacation. We believe that both inpatient and outpatient education benefit when attention is not divided in this way.
Treating the Whole Person
As described on our Mission page, UHPC’s curriculum is guided by the notion that health goes beyond the biological. We address this through multiple facets including:
- Native Hawaiian Health Curriculum
- Patient-Centered Communication Skills Training
- Required experiences in Addiction Medicine and Geriatrics
- Experiences and training in immigrant health and interpreter use
- Exposure to team-based care including social work, mental health, and others
Native Hawaiian Health Curriculum
We are fortunate to have access to great expertise in indigenous health. Our longitudinal curriculum will be designed in collaboration with UH JABSOM’s Native Hawaiian Health Center of Excellence. We will also interface with the Queen’s Medical Center’s Department of Native Hawaiian Health.
Residents will be trained in this field through a combination of didactics, service learning, and clinical experiences. Concepts to be emphasized will include indigenous health models (i.e. lokahi), the importance of sense of place and connection to ‘aina (land) and its history, the importance of ancestry, and the value of storytelling.
These experiences contribute to both the skills our physicians need in the clinic, as well as those of self-care and meaning-making that are vital to a primary care physician’s longterm thriving.
A Broad Definition of Scholarship
All residents are required to complete a mentored, scholarly project. At UHPC, we espouse a modern, broad definition of scholarship, giving residents the freedom to explore fields including:
- Medical Education
- Quality Improvement
- Population Health
- Informatics
- Advocacy
- Medical Humanities
All residents will be guided to submit their work to one or more peer-reviewed forums by their third year.
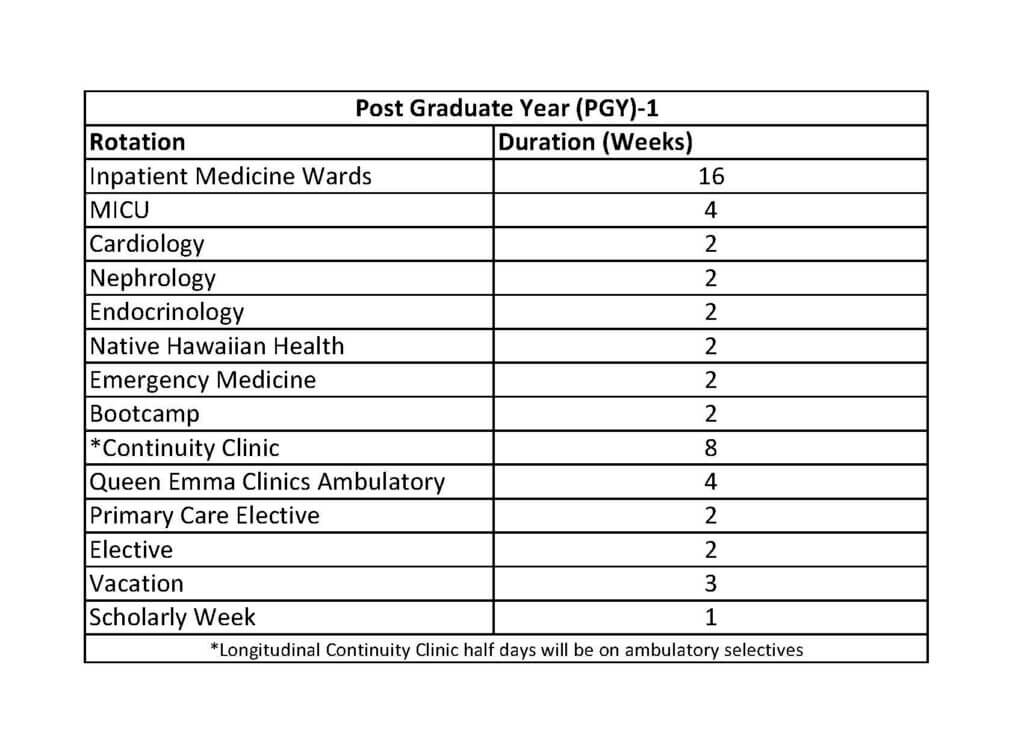
Rotation Schedule


Queen’s University Medical Group Primary Care
UH Primary Care residents will call this site home. Here they will receive a legitimate and longitudinal continuity clinic experience, in which each residents will be assigned as the primary care provider for a panel of patients, while the supervising faculty emphasize graduated autonomy and a sense of ownership and responsibility for the patient panel. This will include responsibility to follow up test results, correspond with care team members and specialists, and respond to patient calls and electronic messages. Residents will also gain significant exposure to the business of medicine by working with attendings and clinic staff to learn about physician payment models (including fee-for-service and payment transformation reimbursement), billing, clinic workflow models, and care coordination.
Rural Health & Neighbor Island Sites
The Rural health preceptorship is an opportunity for UHPC residents to experience thriving primary care practices across the state of Hawai‘i. Residents will spend four weeks in the second year and 4 weeks in the third year at these sites.
- Kihei-Wailea Medical Center, Kihei, Maui – Please see the KWMC Website for more details.
- Hui Kahu Malama, Hilo, Hawai‘i Island – Please see the Hui Kahu Malama Website for more details.
- “Private Ambulatory” and Additional O‘ahu Sites – In addition to continuity clinic at QUMG and neighbor island sites, residents will spend time across a menu of other clinical sites on O‘ahu, such as during the two-week “private ambulatory” rotations in the second and third year, as well as other opportunities throughout the three years.
Clinical Sites
- Queen Emma Clinics – Originally established in 1947 as a government-subsidized clinic providing medical services to those who were unable to pay for care, the vision of QEC lies in aiding Hawai‘i’s underserved communities. The clinic specializes in offering care to those under Hawai‘i’s Med-Quest program, Medicare, or Medicaid programs while also assisting many uninsured patients. Functioning as a multi-specialty department, residents gain exposure to Adult medicine in addition to Cardiology, Dermatology, Endocrinology, Gastroenterology, Gynecology, HIV medicine, Nephrology, Pulmonology, Psychiatry, and Sports medicine clinics. Please see the Queen Emma Clinics website for more details.
- Pearl City Medical Associates – Founded in 1957, PCMA is a primary care group practice with teaching affiliations with the University of Hawai‘i John A. Burns School of Medicine. Located in Waimalu of Central Oahu, PCMA offers a unique experience into a successful private practice with diverse patients representing a cross-section of Hawai‘i’s general population. Please see the PCMA Website for more details.
- Waikiki Health Center – Waikiki Health is a multi-service, multi-site non-profit agency which focuses on providing medical care to underserved populations of Oahu. Originally founded in 1967 as Waikiki Drug Clinic to combat the growing problems of drug addiction, the efforts of this program have expanded to include multiple clinical sites offering Primary care, Preventative medicine, HIV medicine, Women’s Health, Behavioral health, and Dental services. Residents rotate at Waikiki Health Center, a Federally Qualified Health Center (FQHC) which operates as a primary care practice that continues to offer services to patients with general population as well as those with drug addiction, homelessness, and sexually transmitted infections. Please see the WHC Website for more details.
- Queen’s University Medical Group Primary Care – UH Primary Care residents will call this site home. Here they will receive a legitimate and longitudinal continuity clinic experience, in which each residents will be assigned as the primary care provider for a panel of patients, while the supervising faculty emphasize graduated autonomy and a sense of ownership and responsibility for the patient panel. This will include responsibility to follow up test results, correspond with care team members and specialists, and respond to patient calls and electronic messages. Residents will also gain significant exposure to the business of medicine by working with attendings and clinic staff to learn about physician payment models (including fee-for-service and payment transformation reimbursement), billing, clinic workflow models, and care coordination.
- Straub Benioff Medical Center/ Hawai‘i Pacific Health is a not-for-profit health care system, and a site for both Primary Care rotations and sub-specialty medicine electives. Their network of doctors and specialists provides coordinated care that is centered around patients, focusing on prevention, early intervention, monitoring and regular check-ups. At this site, residents will learn about the various resources available within a primary care clinic and integrated sub-specialty practices; and will gain experience caring for the wide range of conditions commonly treated by Internal Medicine physicians in the outpatient setting. Residents will also gain significant exposure to the business of medicine by working with attendings and clinic staff to learn about physician payment models (including fee-for-service and payment transformation reimbursement), billing, clinic workflow models, and care coordination.
Application
The University of Hawai‘i Primary Care Internal Medicine Residency Program (UHPC) will participate in the Electronic Residency Application Service (ERAS)**. In accordance with the NRMP “All-In-Policy,” UHPC will participate “All-In.” We will not offer Pre-Match positions.
UHPC is a relatively NEW and DISTINCT Internal Medicine Program focusing on primary care training. UHPC will be accepting applicants for the 2024-2025 application season. Having its origins as a “track” embedded within the University of Hawai‘i’s categorical Internal Medicine program (UHIMRP), UHPC is now be a “stand-alone” program with the added flexibility and resources to truly enhance and embrace the Primary Care educational experience.
For the 2025 ERAS® cycle, our program strongly encourages all applicants to complete a supplemental ERAS application, offered through the AAMC’s ERAS program. Applicants also will be required to complete the MyERAS application.
The following documents will be reviewed:
- ERAS Application
- Medical School Performance Evaluation (MSPE)
- Personal Statement
- A minimum of two (2) Letters of Recommendation from medicine rotations
- Official Medical School Transcripts
- USMLE or COMLEX Transcripts
International Medical Graduates (IMG) additional requirements:
- Valid certificate from the Educational Commission for Foreign Medical Graduate (ECFMG) or ECFMG Status Report at the time of application. Before the final match you must have attained certificate.
- Must be eligible for a J-1 visa
- For non-social security card holders, must report to Honolulu on June 1st.
- Fluent in spoken and written English
Hawaii Residency Programs, Inc. provides equal employment opportunities to all employees and applicants for employment. We do not discriminate on the basis of age, race, color, religion, gender/sex, national origin, ancestry, citizenship, disability, marital status, domestic or sexual violence victim status, arrest and court record, credit history and credit report, sexual orientation, military and veteran status, or other protects categories in accordance with state and federal laws. If you need accommodations at any time, please contact HRP Human Resources at 808-586-2891.
Salary & Benefits
Contact
University of Hawaii Primary Care Internal Medicine Residency Program
1356 Lusitana Street, 7th Floor
Honolulu, Hawaii 96813
Program Administrator:
Joey Sumulong
Phone: (808) 586-2635
Email: jsumulong@hawaiiresidency.org
Program Director:
James Yess MD, FACP
EMAIL: jyess@hawaii.edu
Associate Program Director:
Bryan Brown, MD, MHS
EMAIL: bbrown3@hawaii.edu