About
The University of Hawai‘i, John A. Burns School of Medicine, Department of Psychiatry (DoP) offers a four-year psychiatry residency training program accredited by the Accreditation Council for Graduate Medical Education (ACGME).
The program provides a balanced and theoretical orientation and offers training in a variety of therapeutic approaches. Because of the multiethnic population of Hawai‘i, the program is particularly interested in the cultural aspects of human behavior, psychopathology and psychiatric practice. The program emphasizes the recognition and analysis of disparities in healthcare, including mental health, and addressing them.
The first year focuses on a combination of psychiatry, neurology and internal medicine and is followed by three years of concentrated psychiatric training. Residents receive a broad supervised clinical experience in the practice of contemporary psychiatry, as well as structured teaching. Individual supervision, didactic seminars, rounds and case conferences are the primary techniques used to convey knowledge, clinical skills and the professional attitudes appropriate for a psychiatrist.
Psychiatry was first organized as a clinical section in the mid-1960s when the University of Hawai‘i created a two-year medical school from existing basic science programs. Walter Char, MD headed the section, assisted by psychiatric practitioners in Honolulu who volunteered their time teaching behavioral science to first and second year medical students.
John McDermott, MD was recruited to develop the section into a medical school department as the school evolved into a full degree granting program. He and Dr. Char created a full four year psychiatry curriculum for medical students, and reorganized the existing one year residency program into the four year psychiatry residency program at the University of Hawai‘i John A. Burns School of Medicine that was originally accredited in April 1965.
The primary mission of the Program is to provide residents with a rich educational experience in a variety of clinical settings. Training residents in the knowledge, skills, attitudes, and clinical judgment needed for the practice of psychiatry as well as teaching them to critically appraise the various schools of thought and approach treatment using evidence based medicine.
The fundamental philosophy on which the program rests is the understanding of human behavior on multiple levels and through integration of biological, psychological, and sociocultural dimensions. Because of the multiethnic population of Hawai‘i, the program is particularly interested in the cultural aspects of human behavior, psychopathology, and psychiatric practice.
To graduate competent psychiatrists who can:
- Evaluate and manage the broad spectrum of psychiatric disorders in a variety of settings.
- Manage emergency psychiatry and acute mental health issues in a multicultural patient population from a variety of socioeconomic backgrounds.
- Assume a wide array of contemporary roles, including clinical services, administration, consultation, teaching, advocacy, policy making and research.
- Provide care within Hawai‘i’s mental health system of care as well as other multicultural settings.
Core Faculty & Staff
The University of Hawai‘i Department of Psychiatry is made up of a skilled and versatile team of faculty physicians with various backgrounds, training and experience who educate the residents and fellows in both the traditional didactic setting and the clinical learning environment while providing quality psychiatric care to the people of Hawai‘i.
Program Details
Rotation Schedule
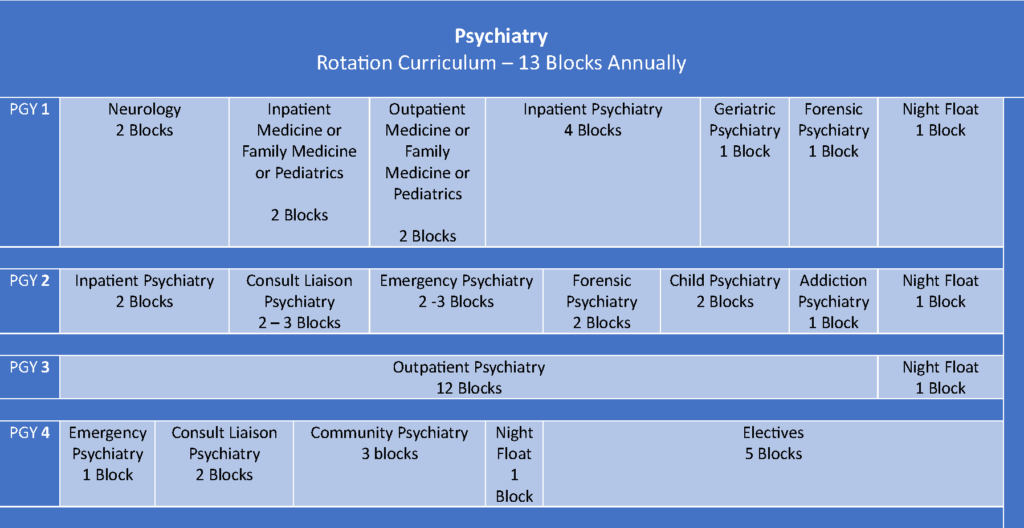
FIRST YEAR
- Inpatient Internal Medicine or Pediatrics (2 blocks)
- Inpatient medicine takes place at the Tripler Army Medical Center or The Queen’s Medical Center, Inpatient Medicine Unit. Residents are part of an internal medicine team and attend medicine didactics while on this rotation. Psychiatry residents are given the same responsibilities as other internal medicine residents, and both follow up on and admit new patients. Rotation usually 6 days/week.
- Pediatric inpatient rotations take place at the Kapi‘olani Medical Center. Residents share similar responsibilities to pediatric residents and are expected to both follow up on admitted patients and help in admitting new patients depending on the type of call day. Residents attend pediatric didactics. Rotation usually 6 days/week.
- Outpatient Internal Medicine or Pediatrics (2 blocks)
- Outpatient medicine takes place at the Pali Momi Outpatient Center or The Queen’s Medical Center, Queen Emma Clinic. Residents work with family medicine residents in seeing patients through their clinic. Residents also see patients in the medical school’s traveling clinic for patients who are homeless. Rotation M-F.
- Outpatient pediatrics takes place at the Kapi‘olani Medical Center. Residents see patients for well-child checks and other acute visits. Rotation M-F.
- Neurology (2 blocks)
- Neurology rotation takes place at the Straub Medical Center. Neurology training is mostly centered in a general neurology clinic where residents both shadow and examine patients presenting with a wide variety of neurological complaints. Residents also follow inpatient neurologists for certain days during the week to gain exposure to more acute neurologic pathologies. Residents occasionally observe pathologists for neuropathology rounds. Rotation M-F.
- Adult Inpatient Psychiatry (6 blocks)
- Inpatient psychiatry training occurs at the Queen’s Medical Center, Kekela Unit. Residents generally carry up to 8 patients. As one of only 2 psychiatric units for non-military affiliated individuals in Hawai‘i, residents gain exposure to working with a multicultural patient population of individuals from Hawai‘i and across the world. Residents work directly with an attending psychiatrist supervisor. Rotation M-F plus 2-3 days/month of Saturday OR Sunday weekend coverage.
- Geriatric psychiatry (1 block)
- Residents work in the Queen’s Medical Center, seeing geriatric patients under the supervision of geriatric medicine physicians. They also visit nursing home(s) and participate in the Queen’s Clinically Integrated Physician Network (QCIPN) on geriatric cases under the supervision of a psychiatrist boarded in geriatric psychiatry. Residents receive training in pharmacologic and behavioral management of disorders ranging from delirium and major neurocognitive disorder with behavioral disturbance to geriatric depression. Rotation M-F.
- Community Psychiatry (1 block)
- This rotation takes place at the O‘ahu Community Correctional Center and the Women’s Community Correctional Center. Residents provide psychopharmacologic management for patients seen in a correctional setting. They also review concepts in forensic evaluation with our forensic psychiatry physicians. Rotation M-F.
- Night Float (1 block per each PGY Level)
- Night Float is completed at the Queen’s Medical Center for one block per PGY Level. Two residents are assigned to complete Night Float together usually pairing an upper with a lower-level resident.
SECOND YEAR
- Addiction Psychiatry (1 block)
- Residents work in various settings including inpatient consultation at the Queen’s Medical Center, local buprenorphine and methadone clinics. All residents must become certified in prescribing buprenorphine during this rotation.
- Child and Adolescent Psychiatry (2 block)
- Residents work with board-certified child and adolescent psychiatrists in the Family Treatment Center at the Queen’s Medical Center. Residents participate in both medication management and family therapy interventions. Residents typically carry up to 4-5 patients and work with children ranging generally from early childhood to adolescence. Residents work M-F with 2 weekends of the month “on call” for new admissions.
- Consult-Liaison Psychiatry (2-3 blocks)
- Residents on the consultation liaison service respond to consultations from the medical and surgical teams at the Queen’s Medical Center. Residents become familiar with a variety of psychiatric and other medical pathologies, refine skills in capacity and safety assessment and gain comfortability in liaising with nursing, social work and primary teams. Residents typically are on duty M-F with 2 half-days of Saturday coverage, Sundays are off.
- Emergency Department Psychiatry (2-3 blocks)
- One of our busier services, residents interview, examine and treat patients who come to the Queen’s Medical Center psychiatric emergency room. We operate as a consult service and provide recommendations for workup, treatment, admission and disposition. Residents refine their skills in triaging and performing emergent safety assessments. Rotation usually 3-4 days/week (2 shifts on 2 shifts off). Shifts are usually 12 hours in duration 8am-8pm.
- Forensic Psychiatry (2 blocks)
- This rotation takes place at the O‘ahu Community Correctional Center. Residents provide psychopharmacologic management for patients seen in a correctional setting. They also review concepts in forensic evaluation with our forensic psychiatry physicians. Other rotation sites include potential away experiences doing forensic evaluations and training at the Hawai‘i State Hospital, a forensic hospital in Hawai‘i. Rotation M-F.
THIRD YEAR
- Outpatient Psychiatry
- PGY-3 residents complete 13 blocks at one of two outpatient psychiatry sites described below that operate Monday-Friday. A half-day per week is dedicated for residents to schedule mandatory psychotherapy supervision. During the year PGY-3 residents will also complete one block of night float and occasional weekend call.
- Queen’s Counseling Services (QCS): Residents see patients referred from the Queen’s Medical Center inpatient, emergency room or consultation liaison settings. Residents at QCS also participate in medication and DBT groups. Weekly didactics occur for training in CBT and IPT. Residents are encouraged to carry at least 3-4 psychotherapy patients but may see more depending on their available schedule. On Wednesdays and Fridays, residents participate in the geriatric psychiatry clinic.
- Veteran’s Administration (VA): Residents at the VA see patients who are veterans or in the military. In addition to seeing medication management and psychotherapy cases, residents also have an opportunity to join multiple groups at the VA. Residents have increased independence on this rotation site and staff their cases once a week with an attending psychiatrist.
- PGY-3 residents complete 13 blocks at one of two outpatient psychiatry sites described below that operate Monday-Friday. A half-day per week is dedicated for residents to schedule mandatory psychotherapy supervision. During the year PGY-3 residents will also complete one block of night float and occasional weekend call.
FOURTH YEAR
- Schedules for fourth year residents are centered around electives, preparing for independent practice in the community and studying for national board examinations using board preparation courses purchased by the program.
- Required rotations in fourth year include ER, CL or Community (Forensics) rotations to prepare for independent practice.
- Residents submit requests in advance of their elective blocks that outline the location, schedule, goals / objectives, milestones, and site supervisor’s approval for review and approval by the Clinical Competency Committee.
- Past electives have included (but are not limited to):
- Addiction Psychiatry
- Administrative Psychiatry (Chief Resident)
- Administrative Psychiatry
- Cultural Psychiatry
- Child and Adolescent Psychiatry
- Community Psychiatry
- Day Treatment
- Electroconvulsive therapy (ECT)
- Emergency Psychiatry
- Forensic Psychiatry
- Group Therapy
- Homeless – Institute for Human Services or Veteran’s Administration
- Geriatric Psychiatry – Nursing Home
- Integrative Medicine
- Integrative Psychiatry / Outpatient Addiction Treatment Program
- Junior Attending Kekela Inpatient
- Medical Student Curriculum Development and Teaching
- Psychopharmacology – Included as part of CL rotation
- Posttraumatic Stress Disorder Psychiatry
- Private Practice with specific practitioners
- Research
- Reproductive Psychiatry
- Telepsychiatry
- Transcranial magnetic stimulation (TMS)
- Electroconvulsant Therapy (ECT)
Call Duties
Resident call duties are designed to offer psychiatric emergency room and overnight psychiatric emergency training experiences. While you will have supervision from an upper-level resident as a PGY-1 and from an attending psychiatrist in all training years, the goal is to build your skills in triaging patients, performing focused psychiatric examinations and safety assessments and your confidence in independent practice.
Call occurs on weekday and weekend evenings. Residents are on-call for no longer than 12 hours per shift (we have no 24-hour call shifts). Call is distributed through a night float system and scattered weekend calls. All call is in-house, with a call room provided.
PGY1
- Weekend calls: none
- Night float: 1 month
- Shifts: 430pm-430am Monday through Friday (with upper-level resident).
PGY2
- Weekend calls: ~6
- Night Float: 1 month
- Shifts: 8pm-8am.
PGY3
- Weekend calls: ~8
- Night Float: 1 month
- Shifts: 8pm-8am.
PGY4
- Weekend calls: 0-maximum of 5
- Night Float: may vary but usually no more than 1-3 weeks
- Shifts: 8pm-8am.
Note on upper resident calls (PGY 2-4): Night float Monday-Friday (with PGY 1 and another upper-level resident). Weekends are solo calls. Weekend calls are not planned for consecutive days (i.e. Saturday and Sunday of the same weekend) unless requested by a resident.
Duties during call:
- Your primary responsibility is treating patients in the psychiatric emergency room.
- Occasionally you may receive calls from the adult or child inpatient unit regarding orders or emergent assessments.
- Emergent consultations from medical floor.
Curriculum
Application
Each year, the University of Hawai‘i Psychiatry Residency Training Program participates in the National Residency Match Program (NRMP) to fill positions. We generally have six (6) to eight (8) PGY-1 positions each year. Applications must be submitted through the Electronic Residency Application Service (ERAS). All applications are reviewed by members of the selection committee only after all documents have been submitted via ERAS.
The following documents are needed to complete your ERAS application:
- ERAS Application Form
- Personal Statement (outlining the following)
- Who you are
- Reasons you are interested in psychiatry
- Reasons you are interested in our program
- Your personal goals
- At least three (3) letters of recommendation, preferably four (4) with two (2) from psychiatrists
- Dean’s letter / Medical School Performance Evaluation (MSPE)
- Official Medical School Transcript
- Official transcripts demonstrating passing scores for:
- USMLE Steps 1 and 2 and/or
- COMLEX Level 1 and 2
- ECFMG certification (if applicable)
All interviews are conducted virtually. Interviews are by invitation only through ERAS (Thalamus) and invites will be released in about October.
Additional Information:
- All non-U.S. citizens applying to the University of Hawai‘i’s Psychiatry residency program must be eligible for a J-1 visa.
- International Medical Graduates (IMGs), whether foreign-born or American-born, are required to hold the standard Educational Commission for Foreign Medical Graduates (ECFMG) certification. See the ECFMG website for more information.
- Hawaii Residency Programs, Inc. provides equal employment opportunities to all employees and applicants for employment. We do not discriminate on the basis of age, race, color, religion, gender/sex, national origin, ancestry, citizenship, disability, marital status, domestic or sexual violence victim status, arrest and court record, credit history and credit report, sexual orientation, military and veteran status, or other protects categories in accordance with state and federal laws. If you need accommodations at any time, please contact HRP Human Resources at 808-586-2891.
Residents
PGY-1 Residents
Lauren Au, M.D.
Medical School: John A. Burns School of Medicine, University of Hawaii
Qianwei Chen, M.D.
Medical School: Robert Wood Johnson Medical School, Rutgers University
Carly Coleman, M.D.
Medical School: John A. Burns School of Medicine, University of Hawaii
Derek Larson, M.D.
Medical School: John A. Burns School of Medicine, University of Hawaii
Awapuhi Lee, M.D.
Medical School: John A. Burns School of Medicine, University of Hawaii
Kristopher Lin, D.O.
Medical School: Arizona College of Osteopathic Medicine of Midwestern University
Evan Liu, M.D.
Medical School: Rush Medical College of Rush University
Pablo Read, M.D.
Medical School: Creighton University School of Medicine
PGY-2 Residents
Shreya Chadda, D.O.
Medical School: Touro University College of Medicine, California
Angela Hu, M.D.
Medical School: University of Arizona College of Medicine – Phoenix
Kyung Moo Kim, M.D
Medical School: John A. Burns School of Medicine, University of Hawaii
Sean Lee, M.D.
Medical School: University of Texas Medical Branch at Galveston
Daniel Nguyen, M.D.
Medical School: University of California – Davis
Ravjoot Randhawa, M.D.
Medical School: Windsor University School of Medicine
Michelle Stafford, M.D.
Medical School: John A. Burns School of Medicine, University of Hawaii
Kyla Yamashita, M.D.
Medical School: Saint Louis University School of Medicine
PGY-3 Residents
Clark Caballero, M.D.
Medical School: John A. Burns School of Medicine, University of Hawaii
Sean He, M.D.
Medical School: Saint Louis University School of Medicine
Charlene Hsia, M.D
Medical School: Oakland University William Beaumont School of Medicine
Sohee Ki, M.D.
Medical School: Keck School of Medicine of the University of Southern California
Jared Kim, M.D.
Medical School: John A. Burns School of Medicine, University of Hawaii
Christian Krause, M.D.
Medical School: Creighton University School of Medicine
Eryn Nakashima, M.D.
Medical School: John A. Burns School of Medicine, University of Hawaii
Alyssa Peric, M.D.
Medical School: John A. Burns School of Medicine, University of Hawaii
PGY-4 Residents
Ryan Adachi, D.O.
Medical School: Touro University College of Osteopathic Medicine, California
Brian Lammert, M.D.
Medical School: University of Washington School of Medicine
Kyle Still, D.O.
Medical School: Western University of Health Sciences College of Osteopathic Medicine of the Pacific, Lebanon Campus
Bryant Yu, M.D.
Medical School: Rush Medical College of Rush University
Benefits & Salary
Contact
University of Hawaii Psychiatry Residency Programs
1356 Lusitana Street, 4th Floor
Honolulu, Hawaii 96813
Cheryl Halvorson – Program Administrator
Phone: (808) 586-2903
Fax: (808) 586-2940
Email: chalvorson@hawaiiresidency.org