About
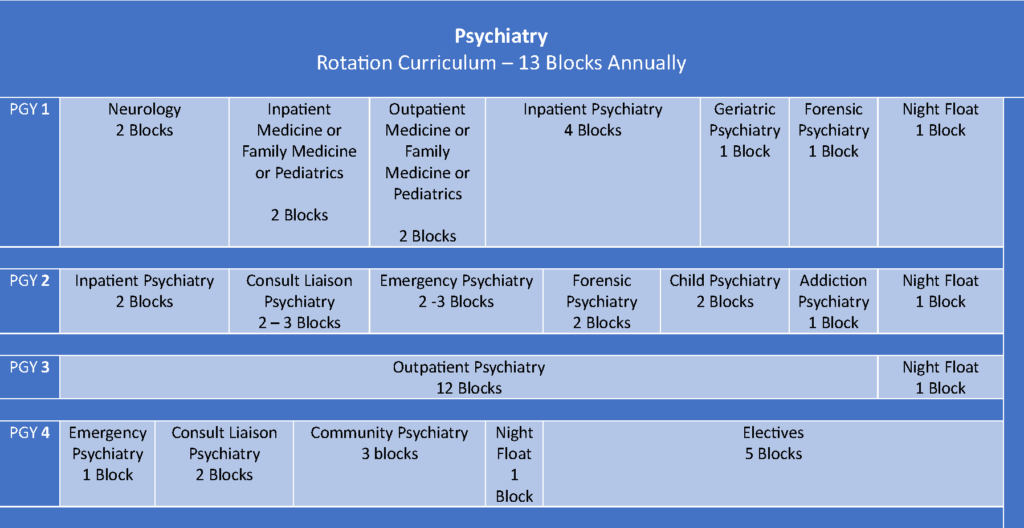
The University of Hawaiʻi, John A. Burns School of Medicine, Department of Psychiatry (DoP) offers a four-year psychiatry residency training program accredited by the Accreditation Council for Graduate Medical Education (ACGME).
The program provides a balanced, diverse, theoretical orientation and offers training in a variety of therapeutic approaches. Because of the multiethnic population of Hawaii, the program is particularly interested in the cultural aspects of human behavior, psychopathology and psychiatric practice. The program emphasizes the recognition and analysis of disparities in healthcare including mental health and addressing these inequalities.
The first year focuses on a combination of psychiatry, neurology and internal medicine and is followed by three years of concentrated psychiatric training. Residents receive a broad supervised clinical experience in the practice of contemporary psychiatry, as well as structured teaching. Individual supervision, didactic seminars, rounds and case conferences are the primary techniques used to convey knowledge, clinical skills and the professional attitudes appropriate for a psychiatrist.
Psychiatry was first organized as a clinical section in the mid-1960s when the University of Hawaii created a two-year medical school from existing basic science programs. Walter Char MD headed the section, assisted by psychiatric practitioners in Honolulu who volunteered their time teaching behavioral science to first and second year medical students.
John McDermott MD was recruited to develop the section into a medical school department as the school evolved into a full degree granting program. He and Dr. Char created a full four year psychiatry curriculum for medical students, and reorganized the existing one year residency program into the four year psychiatry residency program at the University of Hawaii John A. Burns School of Medicine that was originally accredited in April 1965.
The primary mission of the Program is to provide residents with a rich educational experience in a variety of clinical settings. Training residents in the knowledge, skills, attitudes, and clinical judgment needed for the practice of psychiatry as well as teaching them to critically appraise the various schools of thought and approach treatment using evidence based medicine.
The fundamental philosophy on which the program rests is the understanding of human behavior on multiple levels and through integration of biological, psychological, and sociocultural dimensions. Because of the multiethnic population of Hawaii, the program is particularly interested in the cultural aspects of human behavior, psychopathology, and psychiatric practice.
To graduate competent psychiatrists who can:
- Evaluate and manage the broad spectrum of psychiatric disorders in a variety of settings.
- Manage emergency psychiatry and acute mental health issues in an economically and ethnically diverse patient population.
- Assume diverse contemporary roles, including clinical services, administration, consultation, teaching, advocacy, policy making and research.
- Provide care within Hawaii’s mental health system of care as well as other culturally diverse settings.
Core Faculty & Staff
The University of Hawai’i Department of Psychiatry is made up of a diverse team of faculty physicians with various backgrounds, training and experience who educate the residents and fellows in both the traditional didactic setting and the clinical learning environment while providing quality psychiatric care to the people of Hawai’i.